What is the goal of breast reduction?
Breast reduction surgery is performed to address chronic symptoms associated with large breasts and improve breast aesthetics. As a byproduct it simplifies clothing issues and raises self esteem. Patient satisfaction is very high with this procedure despite incurring significant scars in the process.
Will a breast reduction relieve symptoms?
Breast reduction effectively alleviates neck and back pain associated with heavy breasts. While established shoulder grooving from bra straps remains, the associated discomfort is relieved. Rashes under the breasts often resolve following surgery. Posture is improved both from removing excessive breast weight and because of greater self confidence.
Who is a candidate for breast reduction?
Breast reduction can be performed at any age although there are two main groups that seek treatment. Women between fifteen and thirty represent the largest group. Older women who have developed large breasts as a result of weight gain or postmenopausal changes also are candidates. Both groups are effectively treated by breast reduction surgery.
When should breast reduction be performed?
Women who seek breast reduction are typically committed to the idea at a young age. Most are unwavering in their desire despite parental concerns to delay the procedure because of its finality. Overwhelming patient satisfaction with the procedure supports permitting surgery once firm commitment to the idea becomes apparent. Breast size must be stable prior to having surgery, however. Regular menstruation and six months of no breast growth is a reasonable parameter to guide timing in very young women.
What is body mass index (BMI) and why is it important?
Body mass index is a measure that correlates height and weight to categorize weight health. Those with a BMI over 30 are considered obese (Table 1). Medical studies have shown that obese individuals are more prone to surgical complications such as infection and wound healing problems that may require additional surgery. They are also at greater risk from anesthesia. Patients with a BMI over 30 are therefore higher risk candidates for surgery. Weight loss is strongly recommended prior to surgery to reduce this risk.

How is a breast reduction done?
Breast reduction surgery removes skin from the lower part of the breast to gain access to the underlying gland. Breast tissue is then removed mostly from the outer part of the breast, less from the center, and least from the inner aspect. During skin closure the nipple position is pushed upward and the diameter of the areola is reduced. Contrary to a common misconception the nipple and areola are not disconnected from the breast at any time during surgery. Plastic drains are placed prior to final skin closure to draw off fluid produced as a byproduct of the procedure.
What are the different options available?
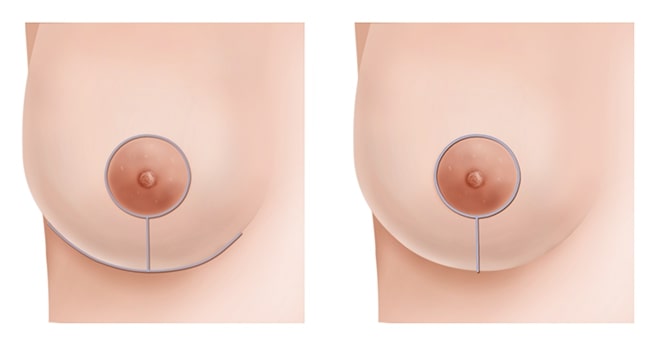
There are two main breast reduction methods. In both types the skin is removed only from the lower part of the breast in order to avoid visible scars above the level of the nipple. The more traditional method of breast reduction leaves an extensive “anchor” scar pattern that includes a scar around the areola, one extending vertically down to the crease under the breast, and a long scar in the crease itself (Figure 1, left). The “lollipop” scar method has fewer scars: only around the circumference of the areola and vertically down to the crease under the breast. There is no scar in the crease itself (Figure 1, right). It is also called a vertical reduction. This method can make wide breasts significantly narrower. It also creates more breast projection compared to the anchor pattern method.
Extremely large breasts that fall as low as the beltline may require a free nipple graft procedure. This is a variation of the anchor pattern method where the nipple and areola actually are completely removed from the breast and implanted in the proper location at the end of the procedure. The nipple and areola has a near normal appearance after surgery but sensation is absent. This method is rarely required.
What do the scars look like?
Scars usually fade considerably by one year. Breast reduction patients are rarely troubled by their appearance. The scars underneath the breasts tend to be the most troublesome in those having the traditional anchor pattern technique. Any scar may spread in response to skin tension no matter how meticulously the closure is performed during surgery. Some individuals normally form scars that are thicker or redder in color than average. It is important to realize that all scars are permanent and their width, texture, and color commonly varies from person to person.
What size will my breasts be after surgery?
The diameter of the breast footprint on the chest wall is a key determinant of bra cup size. Breast reduction does not reduce this dimension in proportion to the amount of tissue removed, however. Therefore it is not possible to accurately predict final cup size following surgery. Most women drop at least one cup size and those who are DD or larger often decrease by two. The emphasis is not to pursue a specific cup size but rather to remove enough tissue to relieve symptoms, raise the breasts as much as possible, and create the best possible shape. Reduction to a B cup in particular is not a realistic request for the vast majority of women.
Will I still need to wear a bra after surgery?
It will remain necessary to wear a bra after breast reduction surgery. However, the bra does not have to work hard to hold the breasts up because a surgical lift has been accomplished as part of the procedure. The bra is more comfortable to wear because it merely holds the breasts in place and masks the nipples.
What about nipple sensation and the ability to breast feed?
Removing breast tissue may cause either a temporary or permanent loss of nipple sensation. The larger the reduction, the greater the likelihood for this to happen. Fortunately, most patients are not affected. Sometimes nipples can become unpleasantly hypersensitive after surgery. This condition typically resolves eventually.
Breast feeding capacity usually remains after a breast reduction. Although the amount of milk producing tissue is reduced, the architecture of the ductal system extending from the remaining tissue into the nipple is preserved. As with the sensation issue, the less tissue removed, the more normal function can be expected after surgery.
How long do the benefits of surgery last?
Women often ask if the results of breast reduction surgery are permanent. It is unlikely that more breast tissue will grow following surgery, except possibly in the very young. However, significant weight gain, multiple pregnancies, and postmenopausal changes can cause the breasts to stretch and enlarge. Despite this, the need for a second procedure is uncommon. Most patients have only one operation and remain pleased.
Where is the surgery performed and how long does it take?
Breast reduction is performed in our office operating room with discharge home the same day. The operation takes from three and one half hours for smaller sizes to as long as five hours or more for very large breasts. The surgery is performed entirely by Dr. Hidalgo.
What type of anesthesia is used?
General anesthesia is required. A board certified anesthesiologist is present for the entire procedure and uses state-of-the-art monitoring equipment.
Can other procedures be done at the same time?
Breast reduction can be combined with other procedures such as eyelid surgery and liposuction of the arms or abdomen. Liposuction limited to one site is the most common adjunctive procedure added because it does not increase total surgery time prohibitively. Most other types of procedures not mentioned are better done separately.
What happens to the tissue that is removed?
Breast tissue removed at surgery is routinely submitted for microscopic examination. The hospital pathology department studies the tissue in detail and issues a report. Significant abnormal findings are fortunately rare.
What are the risks associated with breast reduction?
The most common complication following breast reduction surgery is hematoma, a collection of blood under the skin. This occurs in about one percent of patients. It usually requires return to the operating room on the same day to remove it. Other unusual complications include infection, delayed healing of incisions, excessive scarring, and partial or complete loss of the nipple, the latter extremely rare. A more significant potential problem is the development of leg vein clots (deep venous thrombosis or DVT) that can lead to serious problems such as pulmonary embolism. While very rare, risk factors include age over 40, being overweight, and a previous history of clotting problems. Compression calf boots pump blood through the legs during surgery to reduce risk, as does early ambulation. Fortunately, the vast majority of patients do not have any complications from breast reduction surgery.
Why is smoking so harmful for surgery?
Smoking severely reduces blood supply to the breast tissue and skin. It delays healing and can be responsible for skin and nipple loss, wound infection, bad scars, and other complications that may require corrective surgery. It is therefore essential to stop smoking completely for at least three weeks before surgery and six weeks after surgery. Simply cutting back is not enough. Nicotine containing patches and gum are equally harmful.
What is the recovery like?
Breast reduction surgery is well tolerated largely because the breasts lie essentially outside of the body and superficial to the muscles. Most women describe a burning feeling along the skin incisions and generalized breast discomfort after surgery. Both are well controlled by oral pain medication.
A simple surgical bra that opens in the front is worn for one week. Regular bras with wires can be worn after that. Drains are removed at one week. Skin stitches dissolve and do not require removal.
Most activities that do not involve lifting and carrying heavy items can be resumed after one week, including return to work or school. Flying and driving are not recommended for two weeks. Mild cardiovascular exercise without impact such as a stationary bike can begin gradually at two weeks. More intense exercise can resume at six weeks but activities such as jogging, weightlifting, ball sports, yoga, pilates, skiing, and horseback riding should be delayed for at least two months.
What are the costs involved in having surgery?
There are separate fees for surgery, anesthesia, operating room use, and for analysis of the breast tissue removed. Costs also include preoperative lab tests and medical grade photographs.
Does insurance cover breast reduction?
Insurance coverage of breast reduction surgery is highly variable, depending in part on the insurance company, the type of policy, and the severity of the condition. The more complete the documentation of disabling symptoms before surgery, and the greater the amount of tissue removed at surgery, the more likely that insurance coverage will be approved. The final decision is ultimately at the discretion of the insurance company, however. Preapproval is mandatory today if benefits are to be expected.
What are the steps involved in proceeding with surgery?
At the initial consultation your breast anatomy will be evaluated and a specific surgical plan proposed, provided that you are a good candidate for one of the available options. Once the plan is agreed upon a surgical date can be scheduled. Photographs and preoperative laboratory studies follow. Patients significantly overweight must lose enough weight to bring their body mass index (BMI) measurement to a value of not more than thirty. Women over forty, or those over thirty-five with a family history of breast cancer, should have a mammogram prior to surgery if it has been over a year from the previous study.